What is cancer?
Cancer is a collection of diseases characterized by uncontrolled cell replication and growth.[1] Solid cancers form a harmful tumor from a specific type of tissue, while hematological (blood) cancers form from lymphatic and blood tissues.[2] As cancers grow, they become more malignant, and the most advanced cancers spread to other areas of the body in a process called metastasis. Some types of cancer can be treated with a high margin of success, while other cancers usually lead to death.[3]
How could diet affect cancer?
Epidemiological studies suggest that dietary patterns are a large contributor to the global cancer burden and are a key area to focus on for preventing cancer.[4] A number of diet intervention studies confirm the role of diet in cancer risk by looking at markers of cancer risk,[5] but few interventions have actually tested the effect of diet on preventing cancer.[6][7] The majority of dietary interventions focus on either preventing cancer recurrence, slowing progression, or managing the symptoms of cancer and cancer treatments.[8][9][10] Generally speaking, weight management through diet and antioxidant-rich diets are focal points in nutrition for cancer research.
Which supplements are the most studied for cancer?
Some examples of well-studied herbal supplements in the context of cancer are traditional Eastern herbal medicines, garlic, caffeine, guarana, spearmint and peppermint. A decades-old body of research also points to the use of cannabis and CBD for managing symptoms of cancer treatment. Vitamins and nutrients that have been thoroughly studied include vitamin D, vitamin E, vitamin C, vitamin A and beta-carotene, selenium, zinc, and combinations of these vitamins. Supplements that may improve gut health symptoms caused by cancer treatment include glutamine, probiotics, ginger, short-chain fatty acids, proteolytic enzymes, kefir, honey, and propolis, among many others.
Examine Database: Cancer
Research FeedRead all studies
In this meta-analysis of randomized controlled trials, low-dose aspirin reduced the recurrence of colorectal adenoma among adult participants with a history of adenomas (but no history of colorectal cancer).
Frequently asked questions
Cancer is a collection of diseases characterized by uncontrolled cell replication and growth.[1] Solid cancers form a harmful tumor from a specific type of tissue, while hematological (blood) cancers form from lymphatic and blood tissues.[2] As cancers grow, they become more malignant, and the most advanced cancers spread to other areas of the body in a process called metastasis. Some types of cancer can be treated with a high margin of success, while other cancers usually lead to death.[3]
Despite affecting 1 in 6 people and ranking high on causes of mortality globally, 33–50% of deaths from cancer are from outcomes caused by modifiable behaviors. Some chronic infections are risk factors for cancer, which is a particularly important issue for prevention efforts.[11]
Cancer risk increases due to controllable and uncontrollable factors. Often, a specific risk factor increases risk for a specific type of cancer. Behavioral risk factors include tobacco use, excess alcohol consumption, poor quality dietary patterns, obesity (with caveats), lack of physical activity, and excessive UV radiation. Other modifiable risk factors include viral infection (i.e. HPV) and environmental exposures like aflatoxin and air pollution).[11] Some risk factors for cancer cannot be changed. Few genetic mutations cause cancer, but many genetic mutations interact with other exposures to increase or decrease cancer risk. This is called the “two-hit hypothesis”.[12]
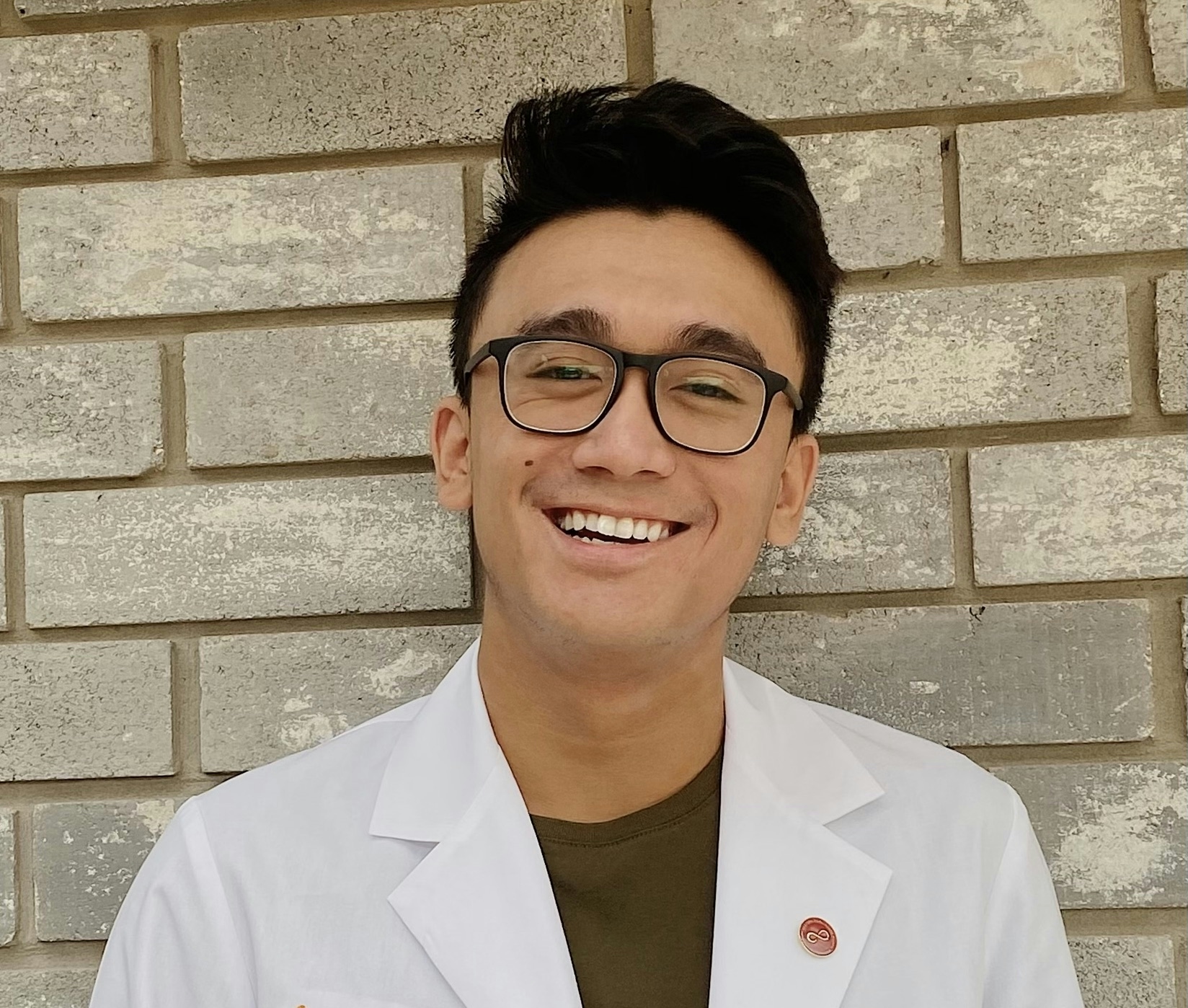
Hematologists are physicians who specialize in blood based cancers. Oncologists deal with solid tumor cancers. Radiologists specialize in radiation treatment. Surgeons specialize in surgical treatments. Medical oncologists specialize in chemotherapy, hormone therapy, biologics therapy, and immunotherapies.
Epidemiological studies suggest that dietary patterns are a large contributor to the global cancer burden and are a key area to focus on for preventing cancer.[4] A number of diet intervention studies confirm the role of diet in cancer risk by looking at markers of cancer risk,[5] but few interventions have actually tested the effect of diet on preventing cancer.[6][7] The majority of dietary interventions focus on either preventing cancer recurrence, slowing progression, or managing the symptoms of cancer and cancer treatments.[8][9][10] Generally speaking, weight management through diet and antioxidant-rich diets are focal points in nutrition for cancer research.
You may have read the headlines that red meat causes cancer. We investigated the actual science.
On a population wide basis, red meat is definitely associated with cancer. The association has been shown numerous times, but is fairly weak in relevance. The most well-controlled study noted an 0.2-fold increase.
Please note association; this has not yet been shown through interventions nor is the cause known. If we are to answer 'does red meat cause cancer', the answer is 'we do not know'
Epidemiology
Recently, a study published controlled for other dietary confounders as well as activity and the basics (smoking, alcohol, social class) and found a Hazard Ratio of 1.16 (+16% risk) for red meat and cancer.[35] Past studies of the same manner find Hazard ratios around 1.2 as well,[36] although this latter study was criticized for its controls.[37] It should be noted that the 20% increased risk was derived from comparing the top quintile (20%) against the bottom quintile of meat consumption, and means a 0.2-fold increase.
A select few studies look at risk of cancer in general, whereas others look at specific forms of cancer. This is due to red meat intake being weakly but confidently associated with various forms of cancer.[38]
A netherlands cohort found an association with a hazard ratio of 2.66 for unprocessed red meat and 3.47 in regards to esophageal squamous cell carcinoma risk in men.[39] No association was found with gastric cancers or esophageal adenocarcinoma, nor esophageal squamous cell carcinoma risk in women.
Colorectal cancer risk is associated with inactivity and low plant consumption[40]
Some studies that measure fiber intake do not find a strong association with distal colorectal cancer risk and red meat.[41]
Interestingly, chicken skin and eggs have been found to confer more risk than lean meats (in a population of Hawaiins), although the strongest correlation was found with total caloric intake.[42] The Relative Risk ratios tended to not exceed 2.0 overall however.
Difference between processed and unprocessed?
Many studies define 'processed' red meats as those that have had added nitrates, due to the correlation between nitrates in meats and nitrosamine formation in the body.
These meats tend to refer to sausages and hot dogs, bacon and other pink meat such as ham, cold cuts, and croquettes.
Compounding and Contributing factors
Risk of colorectal cancer from red meat rises to an 8.8-fold risk when the subject also smokes, and may be due to carcinogens found in the meats as measured by a preference for well-done meat (higher source of the carcinogens Heterocyclic Amines and Polyaromatic Hydrocarbons).[43]
In persons with overactive NAT1/NAT2 enzymes, there is an increased risk of colorectal cancer from meats.[44][45] This may be due to rapid bioactivation of Heterocyclic Amines, which are known colonic carcinogens. One study noted that this phenotype did not associated with an increased cancer risk (OR=1.43) until HCA intake was measured (OR=6.50); those without the phenotype had a lesser increase in risk (OR=2.32).[46] Other P450 enzymes may also contribute to a lesser extent.[47]
In studies that measure HCAs, they correlate similarly if not better with cancer than red meat does itself.[48][49][50]
As NAT1/NAT2 enzymes metabolize caffeine only after CYP1A, a caffeine tolerance test can be used to assess personal susceptibility to HCA-induced carcinogenesis risk via CYP1A.[51] This has been used in some studies[43] and, informally, might be a good indicator of risk if taken with some skepticism (with more caffeine tolerance correlating with more risk).
Compounding factors tend to be unhealthy habits like smoking and alcohol; things that are either pro-oxidant in nature or interact with liver enzymes
Standard correlations
Many studies note that people who consume more red meat also tend to consume more energy overall and have a higher BMI, eat less fruits and vegetables, and have higher rates of smoking and alcohol consumption with a slightly lower education level.[39][35] Socioeconomic class has also been related to red meat and mortality (lower socioeconomic classes eat more red meat) but this does not seem to fully explain the link either.[52] Exercise is also a factor to be considered, specifically cardiorespiratory fitness, as an indicator of diet.[53]
If not otherwise controlled for, these common confounders can influence the results of survey research.
Causation or Causes?
As there have been no interventions, it cannot be concluded that red meat causes cancer or mortality. It is associated, but causation has not yet been established.
If it were to cause cancer or increased mortality, suspect areas could be as follows.
Meat mutagens
Various compounds produced in meats during cooking and processing have possible pro-carcinogenic effects when consumed by humans. T
The content of HCAs and PAHs are more indicative of preparation method than of meat selected, and tend to be associated with preparation methods of red meats rather than chicken or fish (barbecuing, flame grilling). Nitrosamines tend to be associated with pink meats such as ham or bacon, although their levels are even higher in fermented fish products.
Prevention Techniques?
In all studies that controlled for vegetable intake, a greater risk was seen in people not consuming vegetables. On a whole, vegetable intake seems to confer a protective effect.[35][39] In addition, one research group noted that although red meat causes increases in a variety of cancers[38] that fruits and veggies seemed to confer protective effects against just as wide a variety, and were more protective in cohorts that were more at risk.[54] Fruits appeared to be more protective than vegetables in this study.
Processed meat products are associated with cancer and mortality in survey research, but to a small degree. They are likely unhealthy, technically speaking, but the increase in mortality/cancer is overblown.
Processed meat, in the following sections, tends to refer to pink and cured meat products that use the preservative sodium nitrate. This extends to hams, hot dogs, bacon products, and various pre-packaged deli meats.
Although there are similarities between red meat products and processed meats, the minor differences include cooking possibly making carcinogens and processed meat having a higher nitrate content
Survey Research
In the following sections, hazard ratios (HRs) and confidence intervals (CIs) are used. A hazard ratio is a simple way of demonstrating the increased risk (usually by comparing one group against another defined group, such as high meat intake against no meat intake) and while 1.00 means no significant difference, 2.00 is a doubling and 4.00 a quadrupling while 0.50 and 0.25 are a half and quarter; negative values cannot occur, and a hazard ratio of 2-4 as a minimum to show a magnitudal difference is usually desirable (hazard ratios between 1-2 are quite small in magnitude for survey research)
Confidence intervals (almost always set at 95%) are a mathematical way of saying "we are 95% sure that the true value lies in this range". If the range at all crosses the 1.00 point, then the results are not statistically significant regardless of how large the range may be (due to being unable to rule out no change)
Processed Meat and Cancer Occurrence
Processed meat has been associated with an increased risk of cancer (generally referring to all) with hazard ratios of 1.11-1.12 (95% CI of 1.04-1.19 and 1.06-1.19 divided by gender) for the most recent evidence comparing the highest and lowest quintiles against each other.[36] Smaller sample sizes may have hazard ratios in the 2 range (2.14-2.75).[55] Other cancers that have been associated with increased cancer risk include breast (fixed relative risk for every additional 30g was 1.03 with a 95% CI of 1.00-1.06[56]), pancreatic (HR of 1.19 and 95% CI of 1.04-1.36[57]) and a failure to find a relationship with prostate cancer (1.05 and a 95% CI of 0.99-1.12).[58]
In particular, processed meat appears to be associated with increased risk for colorectal cancers, with higher risk than red meat (poultry not associated and fish is protective)[59][60][61] with one meta-analysis of epidemiological research[62] concluding an increased risk of 1.18 (95% CI of 1.10−1.28) for every 50g increase in processed meat consumption; the increase was similar to 100g increases in red meat.
Processed meat intake does appear to be associated with an increased risk of cancer (colorectal cancer is most well known to be associated with processed meat, but seems to be just as much an increased risk as cancer overall). Despite the statistical significance, the effect size is very small
Processed Meat and All-cause Mortality
Consumption of processed meat has been linked to an increase rate of all cause mortality, with the most recent data (448,568 persons, of which 9,861 died from cancer during the study period) noted that processed meat remained associated with an increased risk of all cause mortality after controls were in place, with a calibrated hazard ratio (HR) of 1.18 (95% CI of 1.11-1.25) when comparing an intake of above 160g daily against the reference intake (10-19.9g).[63]
Both dietary deprivation of meat and excessive levels of meat intake appear to be associated with increased risk for death, but the HR was quite low.
Comparisons to other Meats
Although the most recent (and largest) data has failed to find any negative link between red meat and mortality,[63] a result which has been noted elsewhere,[64] some studies do indeed find an association;[65][35][66] all studies seem to use similar controls for the most predictable confounds (caloric intake, obesity, social status, smoking status, etc.) with the only major difference being locale (European data having no association[63] and American data showing a link[35]).
For poultry products, there does not appear to be an increased risk of death (a slight protective effect that becomes statistically insignificant after weighting).[63]
Processed meat and red meat both appear to be associated with increased mortality and death, with processed meat slightly more reliably associated. Both meat categories still have fairly small magnitudes (never surpassing a doubling of risk), and both poultry and fish are not associated with these adverse effects
Sodium Nitrate
Nitrate Sources
Sodium nitrate is a preservative commonly associated with pink or cured meats which contains dietary nitrate, a molecule that has cardioprotective properties but may also convert into a class of molecules known as nitrosamines. In vitro, nitrosamines are known to be carcinogenic. The nitrate found in processed meat products is the same as that from vegetable products, although their biological effects seem to differ.
The nitrates themselves do not differ between sources, and sodium nitrate from processed meat is the same 'nitrate' that is found in vegetables and drinking water
Nitrosamine Formation
Nitrates can 'nitrosylate' other compounds by donating a nitroso group (donating nitric oxide to a molecule to change its structure),[67] and nitrosylating amines (amino acids) will create nitrosamines. 'Nitrosamine' is a categorical term rather than a single molecule, and while there are select nitrosamines that are carcinogenic (cancer causing)[68] some may be inert.
Other products of nitrosylation include S-nitrosothiols and some minerals such as iron from heme (Nitrosyl iron, or FeNO),[69][70] heme being the ring shaped structure in hemoglobin (red blood cells carrier of oxygen) that holds iron in place.
Nitrate can nitrosylate other compounds by binding to them, and when this occurs to amino acids then nitrosamines are formed
Nitrosyl compounds have been detected in the feces of otherwise healthy volunteers following consumption of red or processed meat products, with their production occurring in a fairly dose dependent manner;[71][72] furthermore, a nitroso compound specific DNA adduct (thought to be a reliable biomarker of causing cancer) has been detected in the colon of humans consuming red meat.[73]
Following consumption of processed and red meats, there does appear to be production of nitroso compounds in humans. At least one study has confirmed DNA damage in the colon from this
Heme as Catalyst
Heme is an issue that applies to both processed meats and red meats, but not poultry nor fish products (at least to a concernable degree).
Role of Heme
An observation that has been noted is that white meats (poultry) do not form nitroso compounds following ingestion to the degree that red and processed meats do[74][75] and there are studies that despite finding associations with processed meat and cancer, fail to find any association with poultry.[36]
Currently, it is thought that the higher presence of heme in red meat products relative to white[76][77] is an explanation. It appears that nitric oxide (from sodium nitrate) has affinity for heme and production of nitrosylheme (some sources refer to it as nitrosyl iron) can act as a catalyst for further nitroso compound formation;[78] this is a function not attributed to isolated iron, but to heme containing iron.[76] This product, when detected in the feces, is a predictor of total nitroso formation[69] alongside transit time (longer time to defecation being associated with higher production) and reduced fecal weight (more fecal weight being associated with less production).[72]
Overall, longer exposure times to higher nitroso concentrations appear to dose-dependently increase the risk of forming DNA adducts (a biomarker of DNA damage and thus cancer risk). Without heme, the production rate appears to be quite slow and thus risk is minimized; even at high levels of intake, the epidemiological research does again suggest that while the risk is present it is not dire.
A current theory is that iron from heme (but not free iron from other sources) appears to itself be nitrosylated and then augment production of other nitroso compounds. Thus when nitrates and heme are coingested, production of nitroso compounds is accelerated. It appears to be dose-dependent
It is thought that the presence of heme in a meat product would act as an almost required catalyst for formation of nitroso compounds (implicated both red meat and processed meat), and in this situation only a higher intake of nitrates would lead to dose-dependent increases in nitroso compound formation.
This current theory is in line with the epidemiological evidence that notes that white meat is not associated with any cancer or cardiovascular mortality, that red and processed meat are both implicated (but processed to a slightly higher degree), and that nitrate intake from vegetables (without heme) are very unreliably correlated with harm.
This theory is able to explain the inability of poultry and vegetables to be associated with an increased cancer risk, despite the latter having nitrate content and the former being a meat product
Summation
Processed meats, through a combination of nitrates and heme (neither one alone appearing to be too much of a problem) appear to dose-dependently form carcinogenic nitrosamines. This is a phenomena very well researched in vitro (outside of living systems) and in animal models, with at least one human study noting that DNA damage has occurred in the colon following consumption of processed meat products. Due to the current state of research (survey research showing a connection, but no interventions existing due to ethical complications of possibly giving a human cancer intentionally) and the biological plausibility, it is reasonable to assume that processed meats do cause cancer.
However, in the survey research the hazard ratios and overall risk is fairly small. While this increased risk does exist (in a dose-dependent manner), due to its size it is wholly possible that dietary or supplemental interventions to reduce cancer risk could eliminate the risk. The possibility of one unforeseen or additional variable negating the risk is why low hazard ratios tend not to be used, despite technically being an increased risk
Some examples of well-studied herbal supplements in the context of cancer are traditional Eastern herbal medicines, garlic, caffeine, guarana, spearmint and peppermint. A decades-old body of research also points to the use of cannabis and CBD for managing symptoms of cancer treatment. Vitamins and nutrients that have been thoroughly studied include vitamin D, vitamin E, vitamin C, vitamin A and beta-carotene, selenium, zinc, and combinations of these vitamins. Supplements that may improve gut health symptoms caused by cancer treatment include glutamine, probiotics, ginger, short-chain fatty acids, proteolytic enzymes, kefir, honey, and propolis, among many others.
Recent evidence has linked B vitamins (specifically Vitamin B6 and vitamin-b12) to an increased risk of lung cancer in men, especially in smokers. Here, we analyze the study and interview the lead author, Dr. Theodore Brasky.
B vitamins are common ingredients of multivitamins, of course, but also of energy boosters, such as energy drinks. But while they are best known for their role in energy metabolism,[13] they may play a role in cancer biology through partaking in one-carbon metabolism[14] and thus in methylation reactions and DNA synthesis.
This hypothesis was substantiated in 2015 when a paper published by the New England Journal of Medicine caused a stir by reporting that nicotinamide (a form of vitamin B3 also known as niacinamide) could reduce the rate of new non-melanoma skin cancers.[15]
B vitamins had gained an “anti-cancer” reputation.
Yet it was just one study showing that one form of vitamin B3 could reduce the rate of one type of skin cancer; it didn’t preclude the possibility that some B vitamins could worsen at least some types of cancers.
To look for other possible connections between B vitamin supplementation and cancer, Dr. Theodore Brasky at The Ohio State University, in collaboration with colleagues at the Fred Hutchinson Cancer Research Center and at University of Taipei, performed a large observational study.[16] Since its publication in the Journal of Clinical Oncology, in 2017, this study has taken the supplement world by storm, for it linked the vitamins B6 and B12 each with a 30–40% increase in overall risk of lung cancer in men.
Let’s take a closer look at the study.
Study design
To look for possible connections between B vitamin supplementation and lung cancer, the researchers analyzed data from the 77,000 participants in the VITamins And Lifestyle (VITAL) prospective cohort study.[17] The study itself was designed to look for possible associations between cancer risk and vitamin, mineral, and non-vitamin/non-mineral supplementation.
The researchers chose to focus on the vitamins B6, B12, and B9, which play an important role in the one-carbon pathways and thus are most likely to affect carcinogenesis. The study participants, all residents of the State of Washington aged 50–76 at the beginning of the study, were classified into five groups based on their average daily dose of supplemental B vitamins over the previous 10 years. Statistical techniques were then used to adjust for confounding factors such as age, education, body size, and family history of lung cancer.
What were the results?
When the data were stratified by sex, B6 and B12 as individual supplements were each shown to increase lung cancer risk by 30–40% in men (but not in women).
The greatest risk was found among men with the highest average daily dose of B6 (>20 mg/day was associated with an 82% greater risk) and B12 (>55 mcg/day was associated with a 98% greater risk) over the ten years preceding the study.
When the data were stratified by smoking status, increased risk was associated with smoking. Smokers who had supplemented with high amounts of B6 had nearly three times the risk of developing lung cancer, and those having supplemented with high amounts of B12 had over three times the risk. The study found no association between supplementation and increased risk in either former smokers or recent smokers. As for never-smokers, the paper states they “were excluded from the smoking-stratified analysis because of the low number of participants with incident lung cancer in that group.”
The study showed that long-term supplementation with B6 or B12 increased lung-cancer risk in male current smokers, especially in those supplementing with high dosages of either vitamin.
What is the mechanism?
One-carbon chemical groups lack stability, so they need to be attached to larger molecules in a process called one-carbon metabolism. The vitamins B6, B9,[18] and B12 play an important part in one-carbon metabolism, which in turn plays a crucial part in methylation reactions and nucleotide synthesis.
The nucleus of each of your cells contains your complete DNA. In your DNA is encoded the genetic blueprint for every protein in your body. How then do cells maintain a unique identity? By each reading only certain parts of your DNA, so that only the appropriate genes are turned on at the appropriate time.
For that purpose, sections of your DNA can be “marked” with methyl groups that prevent the expression of nearby genes. This type of epigenetic imprinting is critical to keeping cells normal, healthy, and well behaved. When the process becomes dysfunctional, the wrong genes can be turned on at the wrong times, potentially leading to uncontrolled cell growth — to cancer.
So how would high amounts of B6 or B12 increase cancer risk? We might find some clues in a recent study on DNA methylation,[19] which found that two years of supplementation with 400 mcg of B9 and 500 mcg of B12 changed DNA methylation. Thus, the increase in cancer risk seen in the Brasky study could be caused, in part, by changes in DNA methylation from long-term B vitamin supplementation.
Another curious finding from the Brasky study was that only men saw an increase in cancer risk from B6 or B12 supplementation. Women did not. We know androgens regulate some of the enzymes that participate in one-carbon metabolism,[20] which might explain the difference.
Androgens and the vitamins B6, B9, and B12 interact to play a role in DNA methylation. Since DNA methylation in part determines which genes are activated (or not) at any given time, this could explain the link between long-term B vitamin supplementation and cancer risk in men.
What does this study mean?
The Brasky study was not designed to show causation, but it did reveal a strong correlation between increased risk of lung cancer and long-term B6/B12 supplementation, especially in high doses and among smokers. There are several ways B vitamins may interact with cancer metabolism; more research is needed to determine the exact mechanisms at work. In the meantime, we are left with three takeaways:
Smoking, as you know, causes lung cancer. If you smoke, stop. If you are unable to stop, avoid supplementing with B vitamins for an extended period of time, especially if you are male. Long-term B vitamin supplementation seems to increase cancer risk in male smokers, possibly by potentiating carcinogenesis in precancerous cells in response to the carcinogens in cigarette smoke (which would explain why only current smokers, not former or recent smokers, seem affected).
The effect of B vitamins on non-smokers is still uncertain. In this study, sample sizes for never-smokers were too small to evaluate associations accurately.
Although observational studies cannot show causation, the associations between B vitamins and cancer risk found in this study raise an important point, which is that high-dose, long-term consumption of any supplement can potentially interact with your biochemistry in unexpected ways. Exceeding the recommended, tested doses of even the most healthful micronutrients may not be innocuous.
Q&A with Dr. Theodore Brasky, PhD, lead author of the study
When this study was published, its finding that B vitamin supplements increased cancer risk in men generated a lot of press. But isn’t there some nuance to that finding, especially with regard to smoking habits? What ultimate take-home message can be extracted from the data?
The nuance is sort of centered around the general idea that once you start chopping up data, you lose precision. In epidemiology, our best estimates come from data reflecting the largest sample sizes. Our most cited finding was that long-term, high-dose supplementation of vitamin B6 and long-term, high-dose supplementation of vitamin B12 were each associated with about a doubling of lung-cancer risk in men. This is an entirely true representation of our results. However, when we drilled down further — and thus lost some precision — we found that this twofold increase in risk was an average across different groups of men, some with no increase in risk (men who had never smoked or had stopped smoking at the time the study began), and some with a threefold to fourfold increase in risk (men who smoked at the time the study began).
Here the scientist is left with two possibilities. Is the real finding (a) based on the larger sample size with more precise data? — men who use these supplements have twice the risk of lung cancer as do men who don’t use these supplements; or (b) based on the subgroups within men with less precise results? — men who currently smoke and who use these supplements have three to four times the risk of lung cancer as do men who currently smoke and don’t use these supplements. To me, the take-home message is the latter.
Supplementation dose, frequency, and duration are all important from a biological standpoint. How were those factors taken into account in the design of the study questionnaire? What were the pros and cons of the different ways of using those factors (and others) to identify meaningful associations with lung-cancer risk?
Put simply, we had a number of options. We could analyze separately a given supplement’s frequency of use (i.e., days per week), duration of use (i.e., number of years in the past 10 [our questionnaire only asked about the past 10 years of use]), and most common dose used, or we could combine those data.
Analyzing separately any single aspect removes the influence of the other two, which is, in my view, not ideal. Combining the data gives two additional options. We could determine a cumulative dose over the past 10 years or an average daily dose over the past 10 years. We chose the latter because it’s easier to understand and because it allowed us to compare risks with what might be expected for intakes at the level of a multivitamin taken daily for the same amount of time.
However, the disadvantage of this option — which, I contend, remains better than the alternatives — is that the 10-year, daily-dose calculation equates short-term, high-dose intakes with long-term, lower-dose intakes. The highest category of intake for supplemental B12, for instance, was >55 mcg/day. This is >55 mcg taken daily, on average, over 10 years. For some people, it may actually have been about that amount daily for 10 years, but for most it was shorter-term use at higher doses that averaged out to this level.
Therefore, >55 mcg is not meant to be interpreted as the actual dose that might confer risk. Indeed, most B12 supplements are sold at much, much higher doses. A standard pill from a bottle at the grocery store might contain between 500 and 2,000 mcg, with instructions that it should be taken daily. This is why the comparison to what might be consumed from a multivitamin (100% RDA) comes in handy.
Although the question “Does B vitamin supplementation increase cancer risk?” is straightforward, extracting a solid answer from a given study population is another matter. Epidemiologists like yourself are experts at identifying risk associations within large study populations. At the other end of the spectrum, basic scientists like myself tend to use defined experimental models to identify important cellular/molecular controls that drive disease processes. Could you comment on how epidemiological studies and basic science (i.e., bench research) fit in the big picture of biomedical science? Do you feel they complement each other?
A better scientist than I could probably comment on this with real nuance. I can only give my interpretation, which is, sadly, not based off any firsthand experience with bench science. I once pipetted something, but my assay didn’t run properly. C’est la vie. Looking broadly across disciplines, I can say that epidemiologists and “basic” scientists have a complementary relationship born out of necessity.
Epidemiologists cite rodent studies because in these experiments a lot of the variables can be controlled. The animals are very similar genetically, they’re all fed the same diet (unless it’s a nutrition study), handled the same way, etc. Moreover, we can perform some trials in animals that are considered unethical in humans — exposing rodents to tobacco smoke, for instance. We often see the results of these studies as hypothesis generating because, after all, the animal is a model for the human. People do not, in fact, have fur or tails, and we are much more genetically diverse than rodents purpose bred for disease models. In some instances, animal models are better approximations than others. Mice have estrous cycles rather than menstrual cycles, so some similarities for reproductive cancers are muddied by physiology here. Similarly, a mouse’s prostate gland is structured differently from a man’s; again, models. The idea is the same for work involving cells in petri dishes, although the contrast is starker. On the other hand, from what I’m told by my colleagues in these fields, epidemiologic research, which is predominantly done in an observational manner, is seen as hypothesis generating.
That we all work together towards the same goal is what’s important. Although we definitely give each other grief, epidemiologists appreciate basic scientists for their explanation of biologic mechanisms, and (I’m assuming) basic scientists appreciate epidemiologists for their findings in need of biologic explanation.
The potential links between creatine and cancer are unclear. In general, evidence from in vitro studies and from studies conducted in animals suggests that creatine may have both cancer-suppressive and cancer-promoting properties,[21] whereas evidence from human research suggests a potential protective role of creatine against cancer.
The potential links between creatine and cancer are unclear. In general, evidence from in vitro studies and from studies conducted in animals suggests that creatine may have both cancer-suppressive and cancer-promoting properties.[21]
For example, in mouse models, both creatine and cyclocreatine (a synthetic analog of creatine) have been reported to slow down the rate of growth of subcutaneously implanted tumors.[22][23][24][25][26][27] The potential antitumor effects of cyclocreatine may require the presence of creatine kinase, through which cyclocreatine is converted to phosphocyclocreatine, which, in turn, potentially acts as an energy depleter by trapping ATP that has been released from the cell’s mitochondria or transported into the cell from outside, thereby limiting cancer cell proliferation.[24] However, because the expression of creatine kinase can vary widely depending on the type of tumor, the potential antitumor effects of cyclocreatine may also vary accordingly.[28] The potential antitumor properties of supplemental creatine may be related to its effects on cellular acidosis, inflammation, and oxidative stress,[25][27] as well as on the regulation of antitumor killer T cell immunity.[29]
On the other hand, findings from some studies suggest that creatine may promote invasion and metastasis of certain types of cancer — including colorectal cancer, breast cancer, and pancreatic cancer — through its energy-buffering properties and modulation of cell signaling.[30][31][32]
It’s important to highlight that the above findings are from in vitro and animal research, so their applicability to humans is currently unclear.
The limited available research in humans seems to suggest a potential protective role of creatine against cancer. Specifically, according to a 2023 cross-sectional study that was performed using data from 7,344 US adults who participated in the 2017–2020 National Health and Nutrition Examination Survey (NHANES), a higher intake of dietary creatine was associated with a lower risk of cancer or malignancy, with a 1% reduction in cancer risk for every additional milligram of creatine per kilogram of body mass consumed daily.[33] Moreover, in a 2006 randomized controlled trial, supplementation with creatine in people with colorectal cancer who were undergoing chemotherapy had no effect on muscle mass, muscle function, or quality of life, but improved biomarkers of nutritional status in a subsample of participants that were undergoing less aggressive chemotherapy.[34]
Overall, the available evidence from in vitro and animal studies suggests that creatine may suppress primary tumor growth, but promote invasion and metastasis of some types of tumor, with limited research in humans linking dietary creatine to a lower risk of cancer as well as to some minor protective effects in people undergoing mild chemotherapy for colorectal cancer.
References
- ^Hanahan DHallmarks of Cancer: New Dimensions.Cancer Discov.(2022-01)
- ^Baan RA, Stewart BW, Straif KMechanisms of carcinogenesis: from initiation and promotion to the hallmarksIARC Scientific Publications.(2019)
- ^Djulbegovic B, Kumar A, Soares HP, Hozo I, Bepler G, Clarke M, Bennett CLTreatment success in cancer: new cancer treatment successes identified in phase 3 randomized controlled trials conducted by the National Cancer Institute-sponsored cooperative oncology groups, 1955 to 2006.Arch Intern Med.(2008-Mar-24)
- ^Steven K Clinton, Edward L Giovannucci, Stephen D HurstingThe World Cancer Research Fund/American Institute for Cancer Research Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: Impact and Future DirectionsJ Nutr.(2020 Apr 1)
- ^Egner PA, Chen JG, Wang JB, Wu Y, Sun Y, Lu JH, Zhu J, Zhang YH, Chen YS, Friesen MD, Jacobson LP, Muñoz A, Ng D, Qian GS, Zhu YR, Chen TY, Botting NP, Zhang Q, Fahey JW, Talalay P, Groopman JD, Kensler TWBioavailability of Sulforaphane from two broccoli sprout beverages: results of a short-term, cross-over clinical trial in Qidong, China.Cancer Prev Res (Phila).(2011-Mar)
- ^Chlebowski RT, Aragaki AK, Anderson GL, Pan K, Neuhouser ML, Manson JE, Thomson CA, Mossavar-Rahmani Y, Lane DS, Johnson KC, Wactawski-Wende J, Snetselaar L, Rohan TE, Luo J, Barac A, Prentice RL,Dietary Modification and Breast Cancer Mortality: Long-Term Follow-Up of the Women's Health Initiative Randomized Trial.J Clin Oncol.(2020-05-01)
- ^Mayne ST, Ferrucci LM, Cartmel BLessons learned from randomized clinical trials of micronutrient supplementation for cancer prevention.Annu Rev Nutr.(2012-Aug-21)
- ^Castro-Espin C, Agudo AThe Role of Diet in Prognosis among Cancer Survivors: A Systematic Review and Meta-Analysis of Dietary Patterns and Diet Interventions.Nutrients.(2022-Jan-14)
- ^Maria G Grammatikopoulou, Konstantinos Gkiouras, Stefanos Τ Papageorgiou, Ioannis Myrogiannis, Ioannis Mykoniatis, Theodora Papamitsou, Dimitrios P Bogdanos, Dimitrios G GoulisDietary Factors and Supplements Influencing Prostate Specific-Antigen (PSA) Concentrations in Men with Prostate Cancer and Increased Cancer Risk: An Evidence Analysis Review Based on Randomized Controlled TrialsNutrients.(2020 Sep 29)
- ^Davies NJ, Batehup L, Thomas RThe role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature.Br J Cancer.(2011-Nov-08)
- ^Hyuna Sung, Jacques Ferlay, Rebecca L Siegel, Mathieu Laversanne, Isabelle Soerjomataram, Ahmedin Jemal, Freddie BrayGlobal Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 CountriesCA Cancer J Clin.(2021 May)
- ^Wang LH, Wu CF, Rajasekaran N, Shin YKLoss of Tumor Suppressor Gene Function in Human Cancer: An Overview.Cell Physiol Biochem.(2018)
- ^Depeint F, Bruce WR, Shangari N, Mehta R, O'Brien PJMitochondrial function and toxicity: role of the B vitamin family on mitochondrial energy metabolismChem Biol Interact.(2006 Oct 27)
- ^Selhub JFolate, vitamin B12 and vitamin B6 and one carbon metabolismJ Nutr Health Aging.(2002)
- ^Chen AC, Martin AJ, Choy B, Fernández-Peñas P, Dalziell RA, McKenzie CA, Scolyer RA, Dhillon HM, Vardy JL, Kricker A, St George G, Chinniah N, Halliday GM, Damian DLA Phase 3 Randomized Trial of Nicotinamide for Skin-Cancer ChemopreventionN Engl J Med.(2015 Oct 22)
- ^Brasky TM, White E, Chen CLLong-Term, Supplemental, One-Carbon Metabolism-Related Vitamin B Use in Relation to Lung Cancer Risk in the Vitamins and Lifestyle (VITAL) CohortJ Clin Oncol.(2017 Oct 20)
- ^White E, Patterson RE, Kristal AR, Thornquist M, King I, Shattuck AL, Evans I, Satia-Abouta J, Littman AJ, Potter JDVITamins And Lifestyle cohort study: study design and characteristics of supplement usersAm J Epidemiol.(2004 Jan 1)
- ^Kim YIFolate and colorectal cancer: an evidence-based critical reviewMol Nutr Food Res.(2007 Mar)
- ^Kok DE, Dhonukshe-Rutten RA, Lute C, Heil SG, Uitterlinden AG, van der Velde N, van Meurs JB, van Schoor NM, Hooiveld GJ, de Groot LC, Kampman E, Steegenga WTThe effects of long-term daily folic acid and vitamin B12 supplementation on genome-wide DNA methylation in elderly subjectsClin Epigenetics.(2015 Nov 14)
- ^Corbin JM, Ruiz-Echevarría MJOne-Carbon Metabolism in Prostate Cancer: The Role of Androgen SignalingInt J Mol Sci.(2016 Jul 27)
- ^Zhang L, Bu PThe two sides of creatine in cancer.Trends Cell Biol.(2022-May)
- ^Kornacker M, Schlattner U, Wallimann T, Verneris MR, Negrin RS, Kornacker B, Staratschek-Jox A, Diehl V, Wolf JHodgkin disease-derived cell lines expressing ubiquitous mitochondrial creatine kinase show growth inhibition by cyclocreatine treatment independent of apoptosis.Int J Cancer.(2001-Nov)
- ^Schimmel L, Khandekar VS, Martin KJ, Riera T, Honan C, Shaw DG, Kaddurah-Daouk RThe synthetic phosphagen cyclocreatine phosphate inhibits the growth of a broad spectrum of solid tumors.Anticancer Res.(1996)
- ^Lillie JW, O'Keefe M, Valinski H, Hamlin HA, Varban ML, Kaddurah-Daouk RCyclocreatine (1-carboxymethyl-2-iminoimidazolidine) inhibits growth of a broad spectrum of cancer cells derived from solid tumors.Cancer Res.(1993-Jul-01)
- ^Kristensen CA, Askenasy N, Jain RK, Koretsky APCreatine and cyclocreatine treatment of human colon adenocarcinoma xenografts: 31P and 1H magnetic resonance spectroscopic studies.Br J Cancer.(1999-Jan)
- ^Miller EE, Evans AE, Cohn MInhibition of rate of tumor growth by creatine and cyclocreatine.Proc Natl Acad Sci U S A.(1993-Apr-15)
- ^Campos-Ferraz PL, Gualano B, das Neves W, Andrade IT, Hangai I, Pereira RT, Bezerra RN, Deminice R, Seelaender M, Lancha AHExploratory studies of the potential anti-cancer effects of creatine.Amino Acids.(2016-Aug)
- ^Patra S, Ghosh A, Roy SS, Bera S, Das M, Talukdar D, Ray S, Wallimann T, Ray MA short review on creatine-creatine kinase system in relation to cancer and some experimental results on creatine as adjuvant in cancer therapy.Amino Acids.(2012-Jun)
- ^Di Biase S, Ma X, Wang X, Yu J, Wang YC, Smith DJ, Zhou Y, Li Z, Kim YJ, Clarke N, To A, Yang LCreatine uptake regulates CD8 T cell antitumor immunity.J Exp Med.(2019-Dec-02)
- ^Zhang L, Zhu Z, Yan H, Wang W, Wu Z, Zhang F, Zhang Q, Shi G, Du J, Cai H, Zhang X, Hsu D, Gao P, Piao HL, Chen G, Bu PCreatine promotes cancer metastasis through activation of Smad2/3.Cell Metab.(2021-Jun-01)
- ^Papalazarou V, Zhang T, Paul NR, Juin A, Cantini M, Maddocks ODK, Salmeron-Sanchez M, Machesky LMThe creatine-phosphagen system is mechanoresponsive in pancreatic adenocarcinoma and fuels invasion and metastasis.Nat Metab.(2020-Jan)
- ^Loo JM, Scherl A, Nguyen A, Man FY, Weinberg E, Zeng Z, Saltz L, Paty PB, Tavazoie SFExtracellular metabolic energetics can promote cancer progression.Cell.(2015-Jan-29)
- ^Ostojic SM, Grasaas E, Cvejic JDietary creatine and cancer risk in the U.S. population: NHANES 2017–2020Journal of Functional Foods.(2023 Sep)
- ^Norman K, Stübler D, Baier P, Schütz T, Ocran K, Holm E, Lochs H, Pirlich MEffects of creatine supplementation on nutritional status, muscle function and quality of life in patients with colorectal cancer--a double blind randomised controlled trialClin Nutr.(2006 Aug)
- ^Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, Willett WC, Hu FBRed Meat Consumption and Mortality: Results From 2 Prospective Cohort StudiesArch Intern Med.(2012 Mar 12)
- ^Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin AMeat intake and mortality: a prospective study of over half a million peopleArch Intern Med.(2009 Mar 23)
- ^Higher Red Meat Intake May Be a Marker of Risk, Not a Risk Factor Itself
- ^Aune D, De Stefani E, Ronco A, Boffetta P, Deneo-Pellegrini H, Acosta G, Mendilaharsu MMeat consumption and cancer risk: a case-control study in UruguayAsian Pac J Cancer Prev.(2009 Jul-Sep)
- ^Keszei AP, Schouten LJ, Goldbohm RA, van den Brandt PARed and processed meat consumption and the risk of esophageal and gastric cancer subtypes in The Netherlands Cohort StudyAnn Oncol.(2012 Feb 20)
- ^Arafa MA, Waly MI, Jriesat S, Al Khafajei A, Sallam SDietary and lifestyle characteristics of colorectal cancer in Jordan: a case-control studyAsian Pac J Cancer Prev.(2011)
- ^Williams CD, Satia JA, Adair LS, Stevens J, Galanko J, Keku TO, Sandler RSAssociations of red meat, fat, and protein intake with distal colorectal cancer riskNutr Cancer.(2010)
- ^Le Marchand L, Wilkens LR, Hankin JH, Kolonel LN, Lyu LCA case-control study of diet and colorectal cancer in a multiethnic population in Hawaii (United States): lipids and foods of animal originCancer Causes Control.(1997 Jul)
- ^Le Marchand L, Hankin JH, Pierce LM, Sinha R, Nerurkar PV, Franke AA, Wilkens LR, Kolonel LN, Donlon T, Seifried A, Custer LJ, Lum-Jones A, Chang WWell-done red meat, metabolic phenotypes and colorectal cancer in HawaiiMutat Res.(2002 Sep 30)
- ^Roberts-Thomson IC, Butler WJ, Ryan PMeat, metabolic genotypes and risk for colorectal cancerEur J Cancer Prev.(1999 Jul)
- ^Yeh CC, Sung FC, Tang R, Chang-Chieh CR, Hsieh LLPolymorphisms of cytochrome P450 1A2 and N-acetyltransferase genes, meat consumption, and risk of colorectal cancerDis Colon Rectum.(2009 Jan)
- ^Ishibe N, Sinha R, Hein DW, Kulldorff M, Strickland P, Fretland AJ, Chow WH, Kadlubar FF, Lang NP, Rothman NGenetic polymorphisms in heterocyclic amine metabolism and risk of colorectal adenomasPharmacogenetics.(2002 Mar)
- ^Yoshida K, Osawa K, Kasahara M, Miyaishi A, Nakanishi K, Hayamizu S, Osawa Y, Tsutou A, Tabuchi Y, Shimada E, Tanaka K, Yamamoto M, Takahashi JAssociation of CYP1A1, CYP1A2, GSTM1 and NAT2 gene polymorphisms with colorectal cancer and smokingAsian Pac J Cancer Prev.(2007 Jul-Sep)
- ^Lin J, Forman MR, Wang J, Grossman HB, Chen M, Dinney CP, Hawk ET, Wu XIntake of red meat and heterocyclic amines, metabolic pathway genes and bladder cancer riskInt J Cancer.(2012 Jan 19)
- ^Lam TK, Cross AJ, Consonni D, Randi G, Bagnardi V, Bertazzi PA, Caporaso NE, Sinha R, Subar AF, Landi MTIntakes of red meat, processed meat, and meat mutagens increase lung cancer riskCancer Res.(2009 Feb 1)
- ^De Stefani E, Boffetta P, Deneo-Pellegrini H, Ronco AL, Aune D, Acosta G, Brennan P, Mendilaharsu M, Ferro GMeat intake, meat mutagens and risk of lung cancer in Uruguayan menCancer Causes Control.(2009 Nov)
- ^Lang NP, Butler MA, Massengill J, Lawson M, Stotts RC, Hauer-Jensen M, Kadlubar FFRapid metabolic phenotypes for acetyltransferase and cytochrome P4501A2 and putative exposure to food-borne heterocyclic amines increase the risk for colorectal cancer or polypsCancer Epidemiol Biomarkers Prev.(1994 Dec)
- ^Major JM, Cross AJ, Doubeni CA, Park Y, Lian M, Hollenbeck AR, Schatzkin A, Graubard BI, Sinha RSocioeconomic deprivation impact on meat intake and mortality: NIH-AARP Diet and Health StudyCancer Causes Control.(2011 Dec)
- ^Héroux M, Janssen I, Lam M, Lee DC, Hebert JR, Sui X, Blair SNDietary patterns and the risk of mortality: impact of cardiorespiratory fitnessInt J Epidemiol.(2010 Feb)
- ^Aune D, De Stefani E, Ronco A, Boffetta P, Deneo-Pellegrini H, Acosta G, Mendilaharsu MFruits, vegetables and the risk of cancer: a multisite case-control study in UruguayAsian Pac J Cancer Prev.(2009 Jul-Sep)
- ^De Stefani E, Boffetta P, Ronco AL, Deneo-Pellegrini H, Correa P, Acosta G, Mendilaharsu M, Luaces ME, Silva CProcessed meat consumption and risk of cancer: a multisite case-control study in UruguayBr J Cancer.(2012 Oct 23)
- ^Alexander DD, Morimoto LM, Mink PJ, Cushing CAA review and meta-analysis of red and processed meat consumption and breast cancerNutr Res Rev.(2010 Dec)
- ^Larsson SC, Wolk ARed and processed meat consumption and risk of pancreatic cancer: meta-analysis of prospective studiesBr J Cancer.(2012 Jan 31)
- ^Alexander DD, Mink PJ, Cushing CA, Sceurman BA review and meta-analysis of prospective studies of red and processed meat intake and prostate cancerNutr J.(2010 Nov 2)
- ^Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, Overvad K, Olsen A, Tjønneland A, Clavel F, Boutron-Ruault MC, Kesse E, Boeing H, Bergmann MM, Nieters A, Linseisen J, Trichopoulou A, Trichopoulos D, Tountas Y, Berrino F, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Engeset D, Lund E, Skeie G, Ardanaz E, González C, Navarro C, Quirós JR, Sanchez MJ, Berglund G, Mattisson I, Hallmans G, Palmqvist R, Day NE, Khaw KT, Key TJ, San Joaquin M, Hémon B, Saracci R, Kaaks R, Riboli EMeat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutritionJ Natl Cancer Inst.(2005 Jun 15)
- ^Cross AJ, Leitzmann MF, Gail MH, Hollenbeck AR, Schatzkin A, Sinha RA prospective study of red and processed meat intake in relation to cancer riskPLoS Med.(2007 Dec)
- ^Larsson SC, Wolk AMeat consumption and risk of colorectal cancer: a meta-analysis of prospective studiesInt J Cancer.(2006 Dec 1)
- ^Chan DS, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E, Norat TRed and processed meat and colorectal cancer incidence: meta-analysis of prospective studiesPLoS One.(2011)
- ^Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition
- ^Whiteman D, Muir J, Jones L, Murphy M, Key TDietary questions as determinants of mortality: the OXCHECK experiencePublic Health Nutr.(1999 Dec)
- ^Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study
- ^Kahn HA, Phillips RL, Snowdon DA, Choi WAssociation between reported diet and all-cause mortality. Twenty-one-year follow-up on 27,530 adult Seventh-Day AdventistsAm J Epidemiol.(1984 May)
- ^Chemistry and Biology of N-Nitroso Compounds
- ^Povey AC, Badawi AF, Cooper DP, Hall CN, Harrison KL, Jackson PE, Lees NP, O'Connor PJ, Margison GPDNA alkylation and repair in the large bowel: animal and human studiesJ Nutr.(2002 Nov)
- ^Kuhnle GG, Story GW, Reda T, Mani AR, Moore KP, Lunn JC, Bingham SADiet-induced endogenous formation of nitroso compounds in the GI tractFree Radic Biol Med.(2007 Oct 1)
- ^Kuhnle GG, Bingham SADietary meat, endogenous nitrosation and colorectal cancerBiochem Soc Trans.(2007 Nov)
- ^Joosen AM, Kuhnle GG, Aspinall SM, Barrow TM, Lecommandeur E, Azqueta A, Collins AR, Bingham SAEffect of processed and red meat on endogenous nitrosation and DNA damageCarcinogenesis.(2009 Aug)
- ^Hughes R, Cross AJ, Pollock JR, Bingham SDose-dependent effect of dietary meat on endogenous colonic N-nitrosationCarcinogenesis.(2001 Jan)
- ^Lewin MH, Bailey N, Bandaletova T, Bowman R, Cross AJ, Pollock J, Shuker DE, Bingham SARed meat enhances the colonic formation of the DNA adduct O6-carboxymethyl guanine: implications for colorectal cancer riskCancer Res.(2006 Feb 1)
- ^Cross AJ, Harnly JM, Ferrucci LM, Risch A, Mayne ST, Sinha RDeveloping a heme iron database for meats according to meat type, cooking method and doneness levelFood Nutr Sci.(2012 Jul 1)
- ^Bingham SA, Hughes R, Cross AJEffect of white versus red meat on endogenous N-nitrosation in the human colon and further evidence of a dose responseJ Nutr.(2002 Nov)
- ^Cross AJ, Pollock JR, Bingham SAHaem, not protein or inorganic iron, is responsible for endogenous intestinal N-nitrosation arising from red meatCancer Res.(2003 May 15)
- ^Schwartz S, Ellefson MQuantitative fecal recovery of ingested hemoglobin-heme in blood: comparisons by HemoQuant assay with ingested meat and fishGastroenterology.(1985 Jul)
- ^Reactions of nitrous acid and nitric oxide with porphyrins and haems. Nitrosylhaems as nitrosating agents