Immunity & Infectious Disease
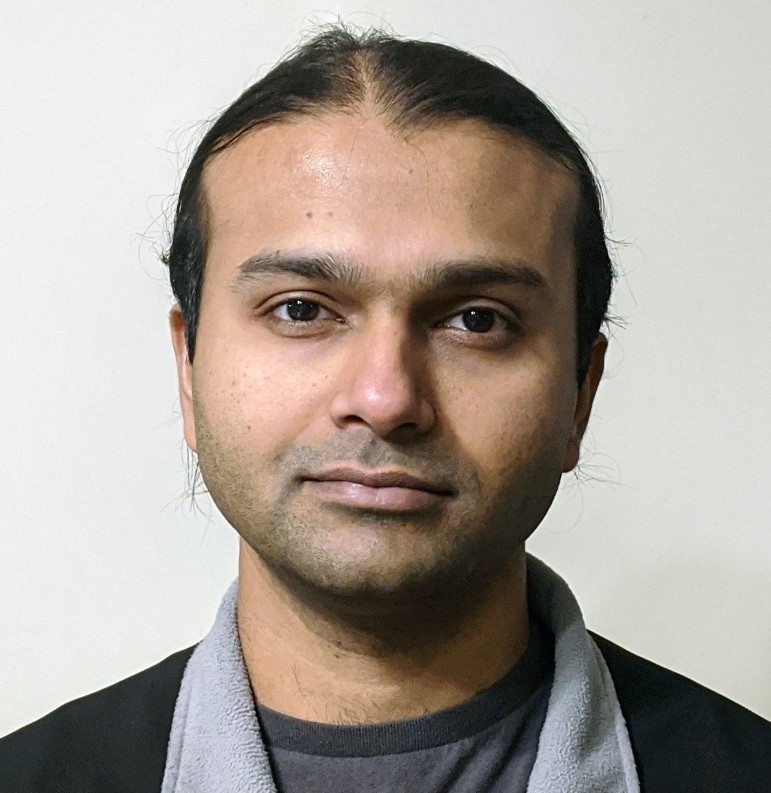
Infectious diseases are caused by microbes, which broadly fall into four categories: bacteria, viruses, fungi, and parasites. Microbes are present in the environment, as well as in and on the human body. The immune system is our body’s defense system against microbes. It differentiates “self” from “nonself” and mounts a response to anything that is foreign to the body.
Last Updated:August 16, 2022
Infectious diseases are human illnesses caused by microbial agents that can be transmitted from one person to another, either through direct contact or through the environment (e.g. infected air, water, food, objects, and surfaces). Some microbes are helpful and are required for normal bodily function, particularly in the gut. Others, under the right conditions, cause human illness. These illnesses range from benign conditions like folliculitis or skin infections, to long-standing and chronic infections (e.g., tuberculosis, leprosy, Lyme disease), to rapidly fatal illness (e.g., SARS, septic shock).
Malnutrition, the inadequate intake of calories and/or protein, is the most common cause of immunodeficiency, which increases the risk of contracting an infectious disease. Similarly, being deficient in certain micronutrients, especially vitamin-a, vitamin-e, vitamin-d, folate, and zinc, increases susceptibility to infections.[1] Consumption of raw, unwashed, inadequately cooked, or contaminated plant material, dairy, or meat is a common mode of acquiring infections from microbes like E. coli, Shigella, Salmonella, Listeria, Campylobacter, hepatitis A virus, norovirus, poliovirus, Giardia, Cryptosporidium, roundworms, pinworms, and tapeworms.
Micronutrient supplementation, specifically vitamin-a, vitamin-e, vitamin-d, folate, and zinc, particularly in the case of specific deficiency, is known to enhance immune infection and reduce susceptibility to different infections. Several herbs, such as garlic, ginger, turmeric, korean red ginseng, licorice, and ashwagandha have shown antiviral and other antimicrobial properties in preclinical studies. Very few have been systematically studied in human clinical studies.[2] In addition, duration, severity and susceptibility to the common-cold are all reduced by garlic supplementation.
Supplement Guide
Click here to read the Allergies & Immunity Supplement Guide- ^Katona P, Katona-Apte JThe interaction between nutrition and infection.Clin Infect Dis.(2008-May-15)
- ^Perera WPRT, Liyanage JA, Dissanayake KGC, Gunathilaka H, Weerakoon WMTDN, Wanigasekara DN, Fernando WSK, Rajapaksha RMH, Liyanage RP, Perera BTAntiviral Potential of Selected Medicinal Herbs and Their Isolated Natural Products.Biomed Res Int.(2021)