Psychedelics and the underlying mechanism of neuroplasticity Original paper
Serotonergic psychedelics exert both cellular and molecular changes in neuroplasticity in preclinical studies. While preliminary clinical studies support these preclinical findings, the use of peripheral sampling and indirect translation of preclinical to clinical research makes it difficult to extrapolate the relevant mechanistic understanding to humans.
This Study Summary was published on December 2, 2021.
Background
Serotonergic psychedelics (psychedelics that primarily act on the 5HT2A receptor) are physiologically safe and can have powerful effects on physiological, cognitive, and emotional states. Various factors, including type, dose, sex, mental state, and environment (setting) can influence how psychedelics affect a person, but it’s been difficult to mechanistically describe how these compounds may exert their lasting effects. This review focuses on the emerging evidence of the effects of psychedelics on neuroplasticity and how these effects may contribute to the benefits of psychedelics.
It’s possible that serotonergic psychedelics may garner some of their positive effects by modulating neuroplasticity. The receptors these drugs bind to can activate signaling pathways that increase neuroplasticity in a variety of ways, such as by increasing neurogenesis and levels of brain-derived neurotrophic factor (BDNF, a protein that plays a crucial role in cell survival and differentiation that is often used as a marker for neuroplasticity).[3][4]
This concept is supported by research showing that stimulation of serotonin receptors by other means increases BDNF. A meta-analysis of 20 clinical trials showed that selective serotonin reuptake inhibitors(SSRIs, a common pharmacological treatment for mental disorders such as depression and anxiety that works in a similar way to serotonergic psychedelics) can increase BDNF levels.[5] Levels of BDNF tend to be lower in people with mental disorders.[6]
The study
This systematic review included 20 experimental studies (16 in animals and 4 in humans) that evaluated the influence of serotonergic psychedelics on neuroplasticity.
The serotonergic psychedelics researchers investigated included ayahuasca, dimethyltryptamine(DMT, or its analog that is quickly degraded into DMT, 5-methoxy-N,N-dimethyltryptamine), lysergic acid diethylamide(LSD), and psilocybin (the bioactive in magic mushrooms).
TABLE 1
| Psychedelic bioactive | Dose | Receptor affinity | Duration | Source |
|---|---|---|---|---|
psilocybin
|
Oral: 0.3–0.6 mg/kg
|
5-hydroxytryptamine (5-HT; AKA serotonin) 1A/B/D/E, 2A/B, 5, 6, 7
|
Start: 10–40 min.; Last: 2–6 hours
|
Psilocybe mushroom species
|
lysergic acid diethylamide (LSD)
|
Oral: 75–150 μg
|
5-HT 1A/D, 2A/B/C, 6; dopamine D1 and D2; alpha-adrenergic receptors
|
Start: 1–2 hours; Last: 6–12 hours
|
Synthesized from naturally-occurring (e.g., ergot fungus Claviceps purpurea) or synthetic precursors
|
| CENTERdimethyltryptamine (DMT)[7]/CENTER |
DMT: 5-HT 1A/D, 2A, 6; 5-MeO-DMT: 5-HT 1A, 2A/B/C
|
Inhaled: 40–50 mg; Oral: Converted into inactive metabolites before sufficient uptake to the brain (i.e., poor bioavailability)
|
Start: seconds to minutes; Last: 15-60 min.
|
Can be chemically synthesized and is even biosynthesized in the brain in amounts that are quickly degraded, but is often extracted from certain plants, such as Psychotropia viridis, and even the toxin of the Colorado River toad.
|
Ayahuasca (DMT + non-psychedelic beta-alkaloids)
|
Oral: 0.6–0.85 mg/kg
|
Similar to DMT, but added alkaloids block monoamine-oxidase (MAO) enzyme activity, which prevents the degradation of neurotransmitters such as serotonin
|
Start: 30 min., Last: up to 4 hours *
|
An extract of Amazonia plants Banisteriopsis caapi (vine containing MAO inhibitors) and Psychotropia viridis (shrub that contains DMT)
|
* longer effects are attributed to MAO inhibition
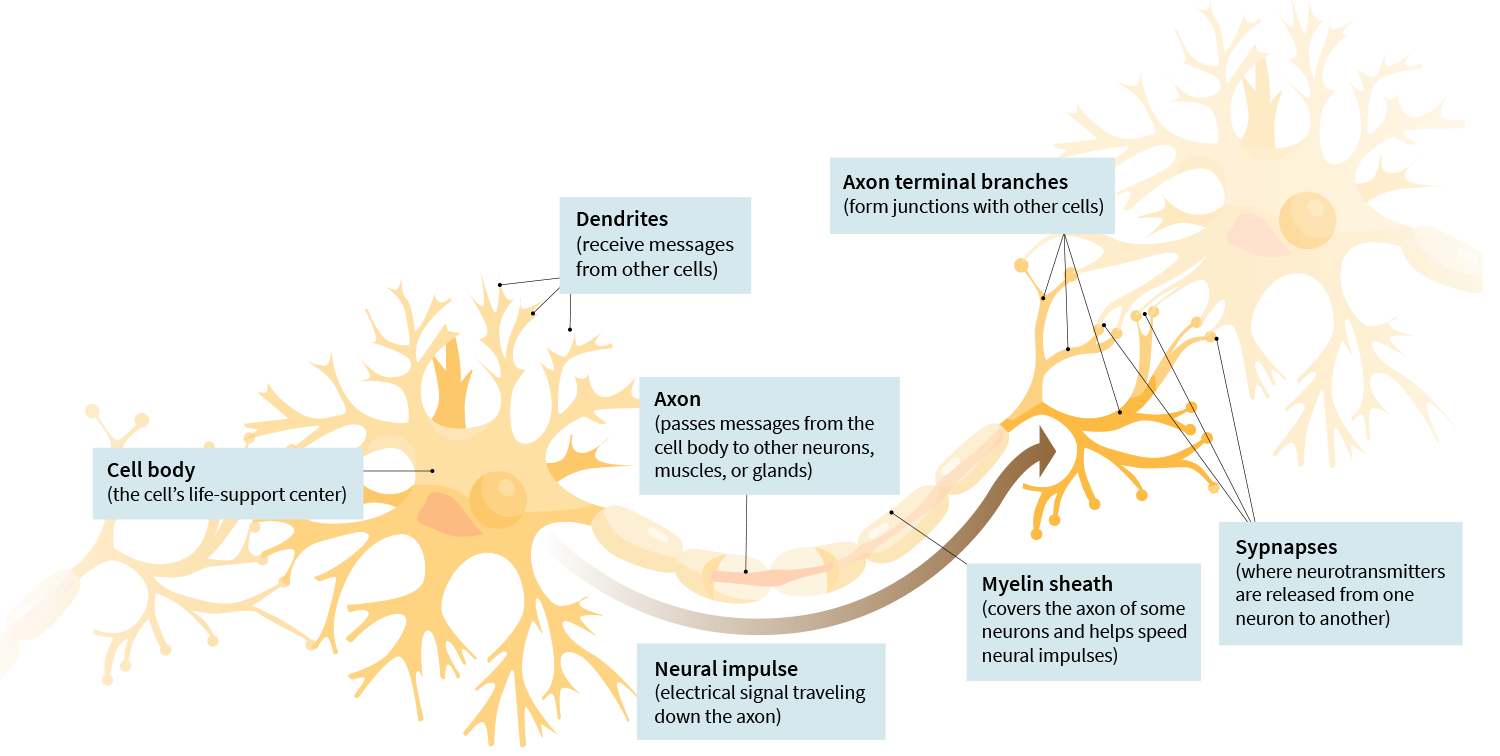
Cellular and molecular neurobiological outcomes included density/number of receptors, dendritic spines, and neurons, along with measures of functional plasticity (i.e., long-term potentiation or depression, indicators of synapse strength related to learning and memory formation) and levels of signaling molecules (e.g., proteins, such as BDNF), receptors, and gene transcription, respectively.
Anatomy of a Neuron
Clinical studies investigated LSD and ayahuasca (2 studies each) and were restricted to questionnaires and serum BDNF measurements.
Researchers evaluated single vs. repeated dose administration, as well as acute (less than 24 hours), subacute (24 hours to 1 week), and long-term effects (more than 1 week).
The results
The preclinical studies show that a single administration of psychedelics acutely stimulates structural neuroplasticity at both molecular (genes and proteins) and cellular (neuronal and dendritic) levels. The four studies that assessed behavioral outcomes showed a seemingly consequential increase in learning behavior. Repeated administration maintained acute neurogenesis and, to a lesser extent, subacute molecular plasticity, as measured by the amount of BDNF produced.
The clinical studies roughly supported the preclinical results for molecular neuroplasticity: increases in BDNF levels correlated with a reduction in depressive symptoms, but BDNF levels did not always change.
Note
Psychedelics are still illegal in many regions, and do not currently have an established therapeutic use in psychiatry, though the scientific literature is building a strong case in support of their therapeutic potential under certain controlled conditions.
Generally, the highest doses administered in clinical studies resemble the lowest doses in preclinical studies that also have small sample sizes (average of about six per group). This makes it difficult to translate preclinical findings to humans and emphasizes the need for human studies with adequate sample sizes that investigate the underlying mechanisms behind psychedelic effects. However, clinical studies tend to report peripheral (blood sample) markers, such as BDNF, that are considered to be less precise than more invasive sampling of cerebrospinal levels of the same molecular neuroplasticity markers.
The big picture
Psychedelic therapy has been proposed as a disease preventive with the potential to cover a range of disorders, assuming adequate therapeutic context, in part due to its plasticity-inducing effects that enhance one’s capacity for change.[8] In the context of maladaptive, reinforced mental habits, psychedelics may serve to break problematic thought patterns by increasing plasticity and capacity for change.
A systematic review involving 17 studies from November 2021 suggests that there may be certain BDNF genetic variants involved in depression, but the relationship is difficult to tease out because there are so many factors involved, such as associations with other genes, disease factors, changes in BDNF levels, and more.[9]
A systematic review of 16 studies demonstrated safety, feasibility, and promising early data for treatment of depression, anxiety, obsessive compulsive disorder, and tobacco and alcohol use disorders with psilocybin, ayahuasca, or LSD.[10] The therapeutic effects in these studies lasted weeks to months after only one to three treatment sessions. Moreover, a meta-analysis of 12 RCTs (covered in a previous Editor’s Pick) demonstrated medium to large effect size improvements in mood disorders (e.g., depression) that also lasted weeks to months, following administration of psilocybin, LSD, or ayahuasca[11].
SSRIs and ketamine, which act on similar receptors, though likely through different mechanisms, have been shown to enhance BDNF levels and synaptic plasticity in association with reductions in symptoms of mental health disorders.[12][5][13][14]
Sex-differences in response to psychedelics[15] and changes in neuroplasticity[16] have been previously observed and may be related to hormonal differences. Estrogen is known to exhibit antidepressant effects through stimulation of BDNF and synaptic plasticity that differs for men and women.[17] This suggests women may have a greater sensitivity to psychedelics.
Get free weekly updates on what’s new at Examine.
This Study Summary was published on December 2, 2021.
References
- ^Pedro Mateos-Aparicio, Antonio Rodríguez-MorenoThe Impact of Studying Brain PlasticityFront Cell Neurosci.(2019 Feb 27)
- ^YouRong Sophie Su, Anand Veeravagu, Gerald Grant, Daniel Laskowitz, Gerald GrantNeuroplasticity after Traumatic Brain Injury.()
- ^Magdalena Miranda, Juan Facundo Morici, María Belén Zanoni, Pedro BekinschteinBrain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological BrainFront Cell Neurosci.(2019 Aug 7)
- ^Antonio Inserra, Danilo De Gregorio, Gabriella GobbiPsychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter MechanismsPharmacol Rev.(2021 Jan)
- ^Chanjuan Zhou, Jiaju Zhong, Bin Zou, Liang Fang, Jianjun Chen, Xiao Deng, Lin Zhang, Xiang Zhao, Zehui Qu, Yang Lei, Ting LeiMeta-analyses of comparative efficacy of antidepressant medications on peripheral BDNF concentration in patients with depressionPLoS One.(2017 Feb 27)
- ^André Russowsky Brunoni, Mariana Lopes, Felipe FregniA systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depressionInt J Neuropsychopharmacol.(2008 Dec)
- ^Steven A BarkerN, N-Dimethyltryptamine (DMT), an Endogenous Hallucinogen: Past, Present, and Future Research to Determine Its Role and FunctionFront Neurosci.(2018 Aug 6)
- ^Rita Kočárová, Jiří Horáček, Robin Carhart-HarrisDoes Psychedelic Therapy Have a Transdiagnostic Action and Prophylactic Potential?Front Psychiatry.(2021 Jul 19)
- ^Manoj K Doss, Michal Považan, Monica D Rosenberg, Nathan D Sepeda, Alan K Davis, Patrick H Finan, Gwenn S Smith, James J Pekar, Peter B Barker, Roland R Griffiths, Frederick S BarrettPsilocybin therapy increases cognitive and neural flexibility in patients with major depressive disorderTransl Psychiatry.(2021 Nov 8)
- ^Kristoffer A A Andersen, Robin Carhart-Harris, David J Nutt, David ErritzoeTherapeutic effects of classic serotonergic psychedelics: A systematic review of modern-era clinical studiesActa Psychiatr Scand.(2021 Feb)
- ^Nicole L Galvão-Coelho, Wolfgang Marx, Maria Gonzalez, Justin Sinclair, Michael de Manincor, Daniel Perkins, Jerome SarrisClassic serotonergic psychedelics for mood and depressive symptoms: a meta-analysis of mood disorder patients and healthy participantsPsychopharmacology (Berl).(2021 Feb)
- ^Carl Björkholm, Lisa M MonteggiaBDNF - a key transducer of antidepressant effectsNeuropharmacology.(2016 Mar)
- ^Carlos A Zarate Jr, Jaskaran B Singh, Paul J Carlson, Nancy E Brutsche, Rezvan Ameli, David A Luckenbaugh, Dennis S Charney, Husseini K ManjiA randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depressionArch Gen Psychiatry.(2006 Aug)
- ^Satoshi Deyama, Ronald S DumanNeurotrophic mechanisms underlying the rapid and sustained antidepressant actions of ketaminePharmacol Biochem Behav.(2020 Jan)
- ^Camila Schoueri Colaço, Stefany Sousa Alves, Luciana Marangni Nolli, Willie Oliveira Pinheiro, Danilo Gustavo Rodrigues de Oliveira, Beatriz Werneck Lopes Santos, Aline Pic-Taylor, Márcia Renata Mortari, Eloisa Dutra CaldasToxicity of ayahuasca after 28 days daily exposure and effects on monoamines and brain-derived neurotrophic factor (BDNF) in brain of Wistar ratsMetab Brain Dis.(2020 Jun)
- ^Alessandra Aparecida Marques, Mário Cesar do Nascimento Bevilaqua, Alberto Morais Pinto da Fonseca, Antonio Egidio Nardi, Sandrine Thuret, Gisele Pereira DiasGender Differences in the Neurobiology of Anxiety: Focus on Adult Hippocampal NeurogenesisNeural Plast.(2016)
- ^Joseph G Oberlander, Catherine S Woolley17β-Estradiol Acutely Potentiates Glutamatergic Synaptic Transmission in the Hippocampus through Distinct Mechanisms in Males and FemalesJ Neurosci.(2016 Mar 2)
