Background
Respiratory tract infections (RTIs) affect parts of the body involved in breathing, such as the nose, throat, or lungs. They’re especially common in the first few years of life.
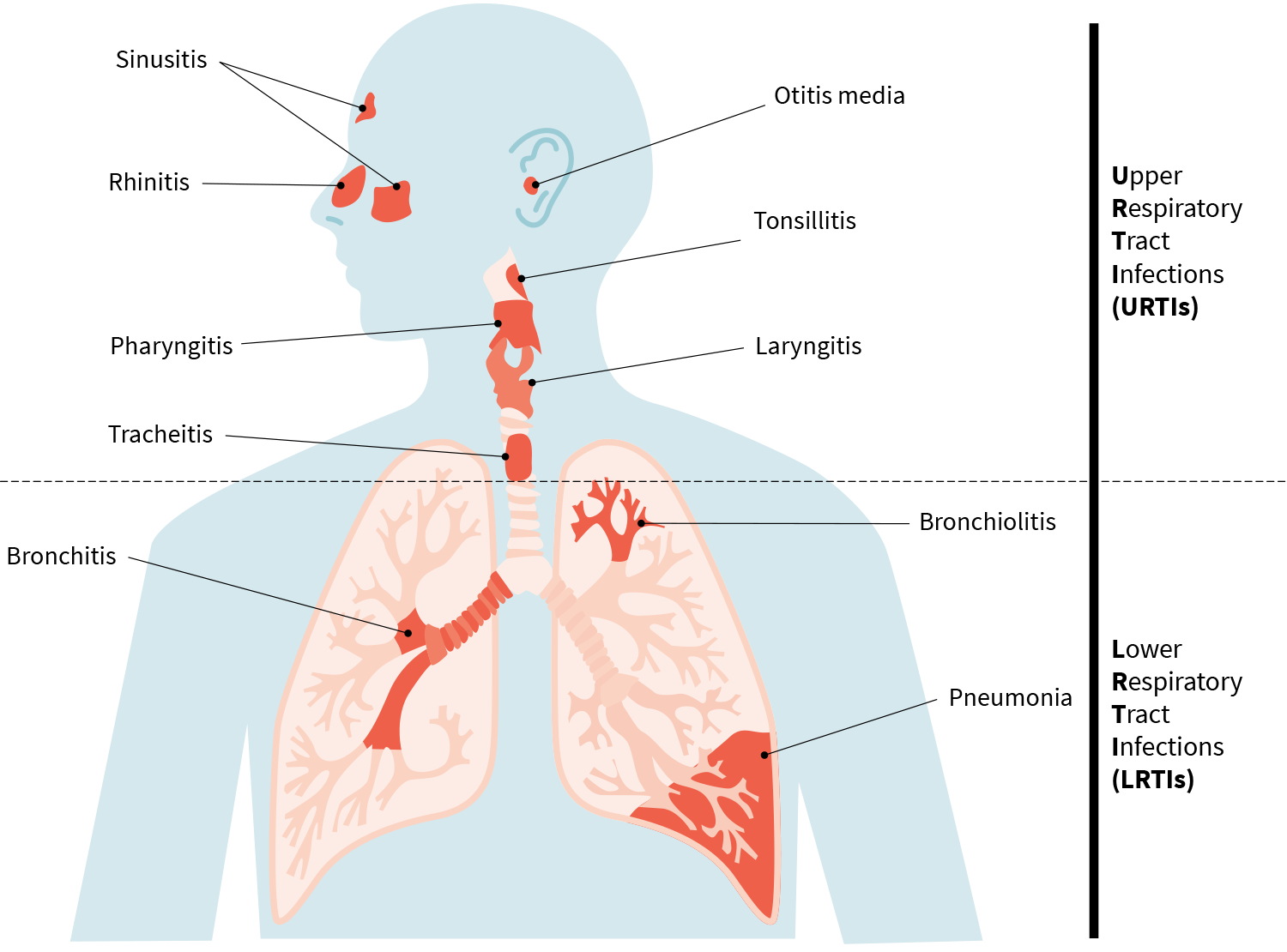
Various types of upper and lower respiratory tract infections
Compared to formula-feeding, breastfeeding has been associated with a lower incidence of RTIs[1] and a healthier gut microflora (less pathogenic bacteria, more Bifidobacteria and Lactobacilli).[2] If the two observations are causally related, then some prebiotics, probiotics, or synbiotics (which combine prebiotics and probiotics) may protect infants against RTIs.
The study
This meta-analysis of 15 randomized controlled trials (RCTs) compared “biotic formulas” (infant formulas containing prebiotics, probiotics, or synbiotics) to control formulas for their effects on the incidence of RTIs. The total 3,805 infants and children were healthy and up to four years old at the start of the interventions, which lasted between three months and five years.
Subgroup analyses were performed based on the type of supplement (prebiotics [7 trials], probiotics [7 trials], and synbiotics [3 trials]) and the type of outcome (upper respiratory tract infections [URTIs; 8 trials], lower respiratory tract infections [LRTIs; 3 trials], and RTIs [8 trials]).
The URTIs were laryngitis, pharyngitis, rhinitis, sinusitis, tonsillitis, tracheitis, and otitis media. The LRTIs were bronchiolitis, bronchitis, and pneumonia. The RTIs involved both URTIs and LRTIs.
The results
In the overall analysis, biotic formulas reduced RTI risk by 11% (compared to control).
In the subgroup analyses, the risk reduction was statistically significant only for RTIs — so not for URTIs, LRTIs, or any of the three types of supplement. (This may be due to the small number of trials in each subgroup rendering the analysis insufficiently powered to detect an effect.)
The methodological quality of all trials was good, and no evidence of publication bias was found.
Note
There was considerable heterogeneity in the main analysis and in most of the subgroup analyses. The trials differed with regard to the type and dose of pre-/pro-/synbiotic, making it difficult to establish an optimal regimen.
The big picture
This was the first meta-analysis to examine the effects of biotic formulas on the incidence of RTIs in infants and young children, but its findings are consistent with those of previous meta-analyses of RCTs examining the effects of probiotics on RTIs.
-
A 2014 meta-analysis looked at children and adults who developed common acute respiratory infectious conditions. It found that probiotics (particularly Bifidobacteria and Lactobacilli) resulted in moderate reductions in sickness duration and total sick days.[3]
-
A 2015 meta-analysis looked at children and adults. It found that probiotics reduced URTI duration, cold-related school absence, antibiotic use, and the number of participants experiencing episodes of acute URTI.[4]
-
A 2016 meta-analysis looked at children. It found that probiotics reduced the number of children with at least one RTI.[5]
-
A 2020 meta-analysis looked at adults. It found that probiotics reduced the incidence, episode rate, and episode duration of URTIs.[6]
You may also be interested in our analysis of a 2016 RCT involving 33 athletes. Of the 16 participants who self-reported a URTI episode, 11 were in the placebo group and 5 in the probiotic group.
This Study Summary was published on January 4, 2022.
References
- ^Liesbeth Duijts, Vincent W V Jaddoe, Albert Hofman, Henriëtte A MollProlonged and exclusive breastfeeding reduces the risk of infectious diseases in infancyPediatrics.(2010 Jul)
- ^Fredrik Bäckhed, Josefine Roswall, Yangqing Peng, Qiang Feng, Huijue Jia, Petia Kovatcheva-Datchary, Yin Li, Yan Xia, Hailiang Xie, Huanzi Zhong, Muhammad Tanweer Khan, Jianfeng Zhang, Junhua Li, Liang Xiao, Jumana Al-Aama, Dongya Zhang, Ying Shiuan Lee, Dorota Kotowska, Camilla Colding, Valentina Tremaroli, Ye Yin, Stefan Bergman, Xun Xu, Lise Madsen, Karsten Kristiansen, Jovanna Dahlgren, Jun WangDynamics and Stabilization of the Human Gut Microbiome during the First Year of LifeCell Host Microbe.(2015 May 13)
- ^Sarah King, Julie Glanville, Mary Ellen Sanders, Anita Fitzgerald, Danielle VarleyEffectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysisBr J Nutr.(2014 Jul 14)
- ^Hao Q, Dong BR, Wu TProbiotics for preventing acute upper respiratory tract infectionsCochrane Database Syst Rev.(2015 Feb 3)
- ^Wang Y, Li X, Ge T, Xiao Y, Liao Y, Cui Y, Zhang Y, Ho W, Yu G, Zhang TProbiotics for prevention and treatment of respiratory tract infections in children: A systematic review and meta-analysis of randomized controlled trialsMedicine (Baltimore).(2016 Aug)
- ^Laodong Li, KangKang Hong, Qixiang Sun, Huan Xiao, Lejin Lai, Moyu Ming, Chaoqian LiProbiotics for Preventing Upper Respiratory Tract Infections in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsEvid Based Complement Alternat Med.(2020 Oct 26)
- ^J Angelin, M KavithaExopolysaccharides from probiotic bacteria and their health potentialInt J Biol Macromol.(2020 Nov 1)
- ^Eric Guillemard, Jérôme Tanguy, Ann'Laure Flavigny, Stephan de la Motte, Juergen SchrezenmeirEffects of consumption of a fermented dairy product containing the probiotic Lactobacillus casei DN-114 001 on common respiratory and gastrointestinal infections in shift workers in a randomized controlled trialJ Am Coll Nutr.(2010 Oct)
- ^Alireza Milajerdi, Seyyed Mohammad Mousavi, Alireza Sadeghi, Asma Salari-Moghaddam, Mohammad Parohan, Bagher Larijani, Ahmad EsmaillzadehThe effect of probiotics on inflammatory biomarkers: a meta-analysis of randomized clinical trialsEur J Nutr.(2020 Mar)
- ^M C Collado, J Meriluoto, S SalminenRole of commercial probiotic strains against human pathogen adhesion to intestinal mucusLett Appl Microbiol.(2007 Oct)