It is possible to exercise yourself into illness. There’s a happy medium where sufficient quantities of exercise can bestow health benefits, including an optimally functioning immune system. But at the upper end of this spectrum, where extreme or exorbitant amounts of physical activity are undertaken, immune system suppression can be a consequence that leads to increased susceptibility to infection. Particularly, heavy training or competition loads undertaken by athletes can increase the risk of acquiring an upper respiratory tract infection (URTI), which can compromise the nasal cavity, mouth, and throat. URTI is an umbrella term that encompasses many infections that affect the upper respiratory tract. Infection types can include the following: tonsillitis, sinusitis, laryngitis, pharyngitis, the “common cold” (which can be caused by many different viruses), influenza, pertussis, and infectious mononucleosis.
One hypothesis as to why hard-training athletes may be more vulnerable to infection is that exhaustive exercise can create an ‘open window’ in the hours following a training session. In this post-exercise period, many components of the immune system may become depressed. While this effect is short-lived, if high-intensity training occurs frequently (as depicted in Figure 1) it can provide many repeated ‘windows’ for infection to opportunistic bacteria and viruses.

A potential contributing factor to this ‘open window’ is the availability of the amino acid tryptophan. During exercise, particularly of an exhaustive or intense nature, the body will accelerate its catabolism (i.e. breakdown) of tryptophan which may be utilized in energy (ATP) and serotonin production. A depression of tryptophan may be an indicator for a decrease in the body's immunosurveillance capability - the ability for your body to ‘check in’ on its immune functions. Prior data has indicated the gut microbiome can play a role in modulating tryptophan levels. In a study of endurance-trained men, supplementing with a probiotic containing six strains (Bifidobacterium bifidum W23, Bifidobacterium lactis W51, Enterococcus faecium W54, Lactobacillus acidophilus W22, Lactobacillus brevis W63, and Lactococcus lactis W58) attenuated markers of inflammation and intestinal permeability - factors that could bolster immune function. However, tryptophan metabolism was not assessed in that study, so its contribution to this effect could not be estimated.
In the study under review, the investigators sought to answer two questions:
- Does the use of a multi-species probiotic preserve tryptophan levels?
- Are higher tryptophan concentrations associated with a decrease in incidence of URTIs in actively training athletes?
Athletes undertaking intense or prolonged training loads may be more vulnerable to a category of illnesses known as upper respiratory tract infections (URTIs). This vulnerability may be due, in part, to the short-term suppression of some immune system components in the post-exercise window. Levels of serum tryptophan may be used as a marker to assess immune system function. The current study sought to determine if the use of a multi-species probiotic may be able to help fortify tryptophan levels during these intense training periods and stave off URTIs.
Who and what was studied?
Thirty-three healthy, young (on average 27 years old), and well-trained male and female endurance athletes were enrolled into the study. This randomized, double-blinded, placebo-controlled trial assigned 17 participants to the multi-strain probiotic and 16 to the placebo group. Within the probiotic were six strains: Bifidobacterium bifidum W23, Bifidobacterium lactis W51, Enterococcus faecium W54, Lactobacillus acidophilus W22, Lactobacillus brevis W63, and Lactococcus lactis W58. Participants in both groups were instructed to take their supplement every day one hour prior to breakfast for the 12-week duration of the study.
Participants were asked to try and maintain their normal diet during the study and were instructed to avoid taking anything that may unduly influence their immune system or microbiome. Such items included anti-inflammatory drugs, antibiotics, probiotics, dietary supplements such as fish oil, certain vitamins (vitamin C, vitamin E) and minerals (selenium), as well as alcohol consumption (more than 10 and 20 grams for women and men, respectively, per day). Fermented dairy products were not allowed.
Weekly training logs noting modality, frequency, intensity, and volume were recorded in addition to logs noting any illness such as URTI or gastrointestinal complaints or symptoms. Illness symptoms were recorded via self-reported questionnaire that identified the type of symptom (runny nose, cough, fever, etc.) as well as the severity of symptoms (from very light to very severe). If the athlete reported at least one symptom over two consecutive days or more, it was defined as an episode of illness. The incidence of URTI illness episodes was the primary outcome of the study.
Lastly, participants underwent pre- and post-study exercise testing and blood draws. Exercise testing comprised performance tests on a cycle ergometer exercise. Two blood draws, once at rest and once after the exercise test, were taken to analyze levels of serum tryptophan and to assess markers of immune function and activation.
Of note is that the study was co-sponsored by the company Winclove Probiotics, who supplied the probiotic (Ecologic® Performance) used in this experiment. The paper notes that “the founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.”
Thirty-three healthy endurance athletes were recruited to receive a multi-strain probiotic or placebo for 12 weeks. Participants were instructed to maintain their normal diet and to refrain from consuming foods, supplements, and medications that may alter their immune function or microbiome. Logs of training schedules and any symptoms of illness were recorded. Pre- and post-study exercise testing and blood draws were taken.
What were the findings?
Four participants were lost to follow-up (12% dropout rate, 3 from intervention and 1 from control group), leaving the results from 29 participants available for final analysis. Compliance with treatments was very high (greater than 95%). After the 12-week treatment period, there were no major differences between groups in regards to body composition, food intake, and performance measures such as VO2max. While differences in resting energy expenditure were significant between groups at the study’s conclusion, the overall net change was very small from baseline. Of note was that the total training volume between groups was consistently unequal over the course of the study. On average, the probiotic group performed eight hours of training per week, compared to 6.6 hours in the placebo group (which may help to explain the differences seen in resting energy expenditure).
Of the immune system biomarkers investigated, there were none that were significantly different between groups over time. The probiotic did appear to preserve blood concentrations of tryptophan after strenuous exercise, but the effect was not significant between groups. The study was powered to detect a difference in tryptophan concentrations, but still failed to reach statistical significance (although it came close). However, the authors weren't detailed in their power calculation. They didn't explicitly say what effect size they were looking for - which is not optimal, since we have no idea what effect size we can rule out. The changes in tryptophan levels over time can be seen in Figure 2.

During the study, 16 participants (55%) self-reported an URTI episode - 11 on placebo and 5 on probiotics. The pre/post difference between groups was statistically significant.
There were no changes of clinical relevance to body composition, food intake, resting energy expenditure, or performance measures at the end of the trial, even though the probiotic group performed about 1.5 hours more training per week on average. While there was a significant decrease in self-reported URTI events in the probiotic group, the only immune biomarker change of note was a preservation in blood concentrations of tryptophan after strenuous exercise. But this effect was not significant.
What does the study really tell us?
The multi-strain probiotic might reduce the incidence of URTI symptoms in athletes undertaking rigorous training or competition schedules. The strains used in this protocol were not chosen at random, but were formulated based on prior evidence of efficacy on immune health in athletes, ability to make it into and populate the intestinal tract, and their previously researched anti-inflammatory properties.
The study did have a number of notable of limitations. Researchers were not able to calculate the severity of illness symptoms due to the high number of no replies on the survey. So, there is no way to determine if the participants were very ill or just had a bit of a runny nose. Another issue is that these symptoms were self-reported, so it’s not possible to determine whether participants experienced an actual infection because it was not serologically confirmed. Lastly, the outcome for which the study was powered (tryptophan levels) was borderline negative and the authors weren't detailed enough in their power calculation to know what effect size they were looking for.
Lastly, the researchers chose to monitor tryptophan levels due to the influence it has in regulating immune function. A drop in tryptophan can affect downstream immunoregulatory pathways. But monitoring these levels presents a “chicken or the egg” problem. Exercise levels can modulate tryptophan breakdown, but so can bacteria or viruses. So, is it the exercise that decreased tryptophan levels, leaving the body vulnerable to infection, or do pathogens take hold, interfering with tryptophan metabolism, which then increases risk of infections? Is it a bit of both? The researchers acknowledge that “longitudinal research will be needed to clarify causal ordering.” Until then it cannot be said if there is a direct effect between probiotic supplementation and reduced tryptophan breakdown.
The probiotic strains included in the supplement have shown promise in modulating various aspects of immune function when tested individually. Researchers were unable to report the severity of symptoms due to incomplete survey questions and were not able to serologically confirm infections, relying only on self-reported symptoms.
The big picture
A meta-analysis of twenty RCTs comprised of otherwise healthy adults and children found that regular supplementation with probiotics, particularly the Lactobacillus and Bifidobacterium strains, resulted in moderate reductions in incidence of total sick days and a shorter duration of illness. The most recent Cochrane meta-analysis also found statistically significant but, clinically speaking, minor effects in non-athletic populations for reducing URTI episodes, the duration illness, and lower rates of antibiotic use.
There are fewer studies looking specifically at probiotic use in an active athletic population. The present study builds on other well-controlled studies in athletes that have produced results showing a probiotic supplement results in fewer days of URTI illness and lower severity of URTI symptoms. A review looking at the research on an athletic population found that, of the studied that reported on incidence of URTI’s, the majority reported “modest clinical benefits in terms of reduced frequency, severity and/or duration of respiratory … illness.” There were a handful that showed no effect, though. And again, the research in these studies were mostly performed with Lactobacillus and Bifidobacterium probiotic strains. As an added bonus, there was also an observed reduction in gastrointestinal illness while supplementing during periods of high volume training and/or competition.
For the general healthy population, a probiotic comprised mostly of Lactobacillus and Bifidobacterium strains provided modest protection against incidence and severity of URTI’s. Looking specifically at an athletic population undergoing intense training programs, the positive effects are still present but are of minor to moderate efficacy.
Frequently asked questions
Q. Besides probiotics, what are other strategies to support immune function in athletes?
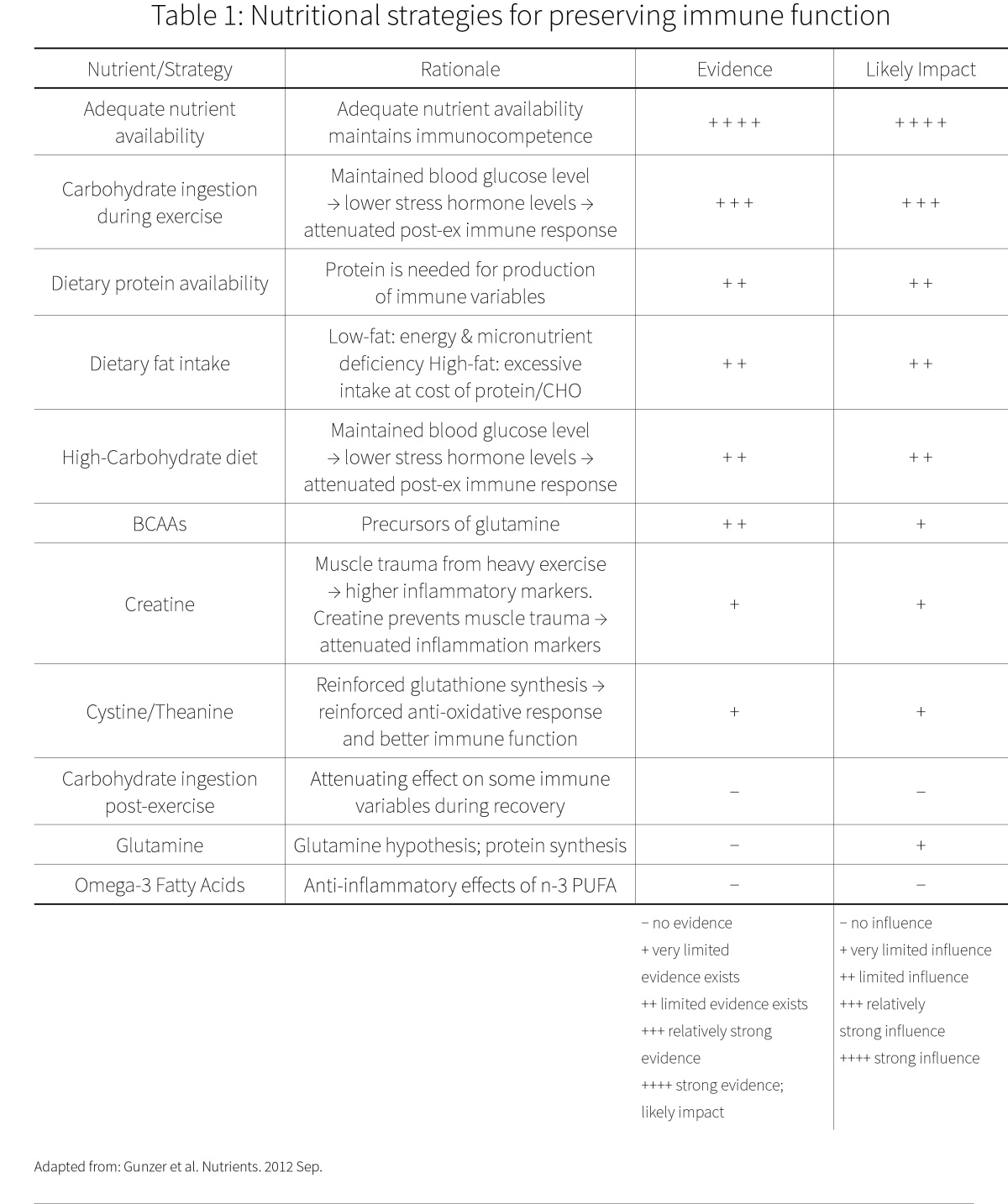
You have probably heard some of these before, but it’s worth repeating! To ensure general support of immune function make sure you are getting sufficient amounts of sleep, eat a varied diet, consume enough calories to support your activity level, and don’t go through extended periods of energy restriction. Additionally, for athletes supplementation with garlic and vitamin C may aid immune function. Keep in mind that garlic will not reduce the duration of a disease or the severity of the symptoms - it is a preventive supplement. Vitamin C might help reduce the duration and severity of colds by a modest amount, but only when taken regularly (i.e. before the first symptoms). Table 1 shows further strategies that have been studied.
Q. Is it necessary to take a multi-strain probiotic to reap these benefits?
The strains in this study were selected because they had shown promise individually in other trials. While these singular strains could provide benefits, a combination might provide a more potent treatment, although we can’t say for sure. However, the mix of probiotics used in this trial has only been tested in two studies. Different bacteria may have quite different uses, such as is shown in Figure 3. Lactobacillus and Bifidobacterium are the two bacteria types that currently have the most research vouching for their efficacy in regards to URTIs.

BONUS: Passionate about probiotics? We got you covered. Here are some further NERD articles that may pique your interest.
- NERD 2 - Of mice and guts (and exercise performance)
- NERD 6 - One pro of probiotic drinks: mitigating harm from overeating
- NERD 7 - Baby probiotics for prevention of ADHD and Asperger’s
- NERD 8 - I get by with a little help from my friends: probiotics and depression
- NERD 13v2 - Probiotics and the propensity for portliness
- NERD 15v2 - Your probiotic may be lying to you
- NERD 16v2 - Little bugs for big depression
- NERD 20v1 - Dead, yet active probiotics?
- NERD 20v2 - Do probiotics alter gut microbiome composition?
- NERD 21v2 - Dampening exam anxiety with probiotics
- NERD 21v2 - Probiotics and prebiotics for atopic dermatitis
- NERD 25v1 - Can probiotics be used to treat multiple sclerosis?
What should I know?
A well-formulated multi-strain probiotic might provide some additional help for reducing URTIs in people who regularly engage in high volumes of exercise. Keep in mind that it may take a few weeks for the full effects to be seen. If you are looking to try supplementing with probiotics for URTI prevention, it would be prudent to try one that contained Lactobacillus and/or Bifidobacterium, as these have the most research for efficacy behind them. However, to have the greatest impact on immune function it would be advisable to ensure you are also getting sufficient sleep and consuming a varied whole-foods based diet.
